This text describes the legal situation in Germany and Switzerland
and is subject to medical quality control.
People who are HIV-positive are not infectious if their treatment is effective.
How safe is treatment as prevention? Does it count as safer sex? Is it more fun? How does this form of prevention work in committed relationships? Does it also work for people who are dating multiple people or during darkroom encounters? What should we do if we are super horny, high, or in love?
CONTENTS
- Treatment as prevention (TasP)
- And is TasP safe?
- How do you get ART?
- Commited Relationships
- Sex dates/Anonymous sex
- Should I out myself as positive before sex?
- A treated future?
- Links and sources
- More info and counseling
- Count on Love Lazers
As people who are HIV-positive and negative, how can we best prevent HIV and other sexually transmitted diseases? Why doesn’t everyone already know about treatment as prevention? Will we manage to reduce discrimination and the exclusion of people living with HIV to an ‘undetectable’ level?
This guide is an attempt to open up a discussion. It’s geared toward men, who have or want to have sex with other men (MSM). Whether you are HIV-negative or positive, trans, bisexual, queer, gay, or simply another type of guy. Furthermore this info is made for trans woman as well. And it’s also for anyone who is just interested.
⇢ Colombia version of this text here
TREATMENT AS PREVENTION (TasP)
This is an HIV prevention method, that is effective when a person who is HIV-positive is successfully treated with antiretroviral therapy (ART). The transmission of HIV during sex is practically impossible if the following conditions are met:
- The person’s viral load is undetectable for 6 months
- Antiretroviral medication (ART) is taken regularly
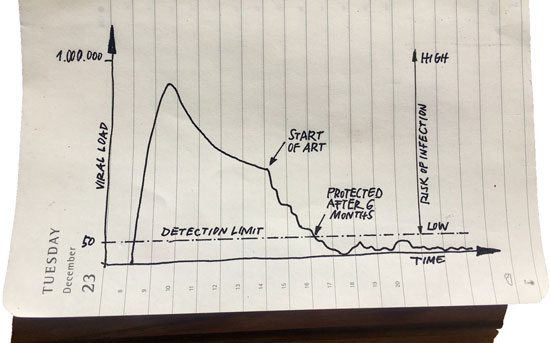
HIV treatment is considered effective, if the multiplication of the virus is suppressed to a level where the virus cannot be detected in the blood by standard testing methods. If this is the case, the individual is then considered “undetectable“. Currently, undetectable means having 50 HIV copies or less per millilitre (ml) of blood. The number of HIV copies per ml is called the “viral load”. This reduces with effective treatment, and after some time, the viral load is also reduced in other body fluids such as sperm.
Regularly taken medication should result in a treatment that is permanently effective, which means that the viral load will remain undetectable. However, blood tests should be done every three months.
Treatment as prevention was first recommended in an official statement made by Swiss AIDS medical practitioners in 2008 as a method for preventing new HIV infections. Based on the state of knowledge of that time, and in particular, with regard to several studies concerning HIV transmission, this “EKAF Statement” or “Swiss Statement” established that people who are HIV-positive are no longer infectious if their viral load is undetectable and if they are regularly taking their medication. They originally claimed that this was true only if no other sexually transmitted infections (STIs) were present however, this is no longer considered to be the case. The treatment works just as well if one has an STI.
This is called, “Treatment as Prevention” or “TasP”. Put simply, a person (actually the virus) is considered undetectable if they have been successfully treated. “U=U” for “Undetectable = Untransmittable” is a worldwide campaign.
AND IS IT SAFE?
Yes, it is safe. There has not been a single documented case in which a new HIV infection has occurred where successful treatment has been undertaken. The results from the PARTNER-Study are clear: there were no HIV transmissions in the 58,000 sexual encounters of 900 heterosexual and homosexual couples. This study confirmed theoretical assumptions, and years of research: where the virus is not present, an infection cannot take place.
However, if the number of viral copies increases (as a result of lapsing treatment or treatment that is working poorly), the risk of infection increases slowly: the more viral copies, the higher the risk of transmission.
Infection through bodily fluids that contain the virus such as blood or sperm did not occur in the aforementioned study when the viral load was less than 200 viral copies/ml. A value under the detection limit (i.e. 50 copies/ml or less) is very safe. Anything below this value is considered safe. Anything above this value is left up to chance.
In the presence of an STI the viral load can slightly increase. However, if treatment is working, that is, if one’s viral load is undetectable, it will always be clearly below the threshold of 200 (viral) copies/ml.
Anyone who has found that their viral load has increased, but has less than 200 (viral) copies/ml while having sex without condoms is very unlikely to have infected anyone. You can stop using condoms or PrEP with a partner, but only once the viral load is permanently below the detection limit (i.e. undetectable).
And what about resistance? When undetectable, HIV viruses that are resistant to medication simply cannot be transmitted. Medication-resistant viruses must therefore be present in a sufficient number to lead to infection.
Incidentally, the consensus today is that the majority of HIV-transmissions occur a few days or weeks after an initial infection. At this time, the individual’s viral load could actually be in the millions, (although an HIV test might still come up negative).
According to the above mentioned studies, treatment as prevention is statistically more effective than the use of condoms. This means, (with regard to HIV) that the current definition of safer sex should be questioned:
Although fucking without a condom (i.e. engaging in bareback sex) is generally thought to be “unsafe”, this is no longer entirely correct.
HOW DO YOU GET ART?
An ART currently consists of several active substances and is paid for by health insurance.
If you test positive for HIV, you will have to make decisions about starting treatment. You should get fully informed about the most optimal way to do this! The best way to get information is at an AIDS support center or from a doctor that specializes in HIV or AIDS.
From the standpoint of prevention, beginning treatment early is a good idea since HIV infections virtually cease to occur under treatment. However, it is up to you to choose the right time: you will have to take the pills every day. Side effects could occur that might be limiting to you. Doctors cannot force you to make any decision about this.
In order for the medications to work effectively, and retain their effects, you must take them regularly. Strict adherence to the ART regimen is called “compliance”, but compliance cannot occur without personal motivation. Remaining compliant means that the viral load can be kept permanently below the detection limit. This can prevent the onset of AIDS and its accompanying symptoms. Successful treatment therefore allows for the lasting preservation of a good quality of life.
Compliance is also a prerequisite for treatment as prevention: you can only remain un-infectious in the long run if you consistently take your medication.
ART is expensive and access to permanent treatment for people without insurance is scarce. In other countries, special funds have been set up to provide HIV medication for people without insurance. This should be demanded from our health care systems. If you need an ART and do not have insurance, speak with your local AIDS organization. They can help clarify what options are available to you.
Those who have applied for asylum are also entitled to financial support for HIV treatment in Germany, (however, this can sometimes be complicated). The practice of deporting someone to a country where treatment cannot be continued is unethical, and condemnable. Everyone who needs treatment or wants treatment as prevention should have access to it, regardless of their situation.
Treatment as prevention is a secondary effect of every HIV-positive individual’s therapeutic success: the more people who are benefitting from it, the greater the preventative benefit there will be for everyone.
COMMITTED RELATIONSHIPS
In discordant couples (with different HIV status), foregoing condoms is now widespread. TasP is recommended to them by various institutions, (such as BAG, BzgA, and Aids-Hilfen).
In 2008, the above-mentioned Swiss (“EKAF”) statement, which was based on various studies, established what had been witnessed for several years: positive people undergoing treatment and not infecting their negative partners, even when they sometimes forgot to use condoms, or when they were deliberately not used (e.g. when they were trying to have children).
Today it is scientifically confirmed that treatment as prevention is actually a simple and proven Safer-Sex method in these types of partnerships, especially when both partners make this decision together.
SEX DATES / ANONYMOUS SEX
There are hardly any official recommendations for treatment as prevention regarding sex dates or anonymous sex. This is likely due to the lack of studies dealing exclusively with sex outside of committed partnerships, and possibly for reasons having to do with certain moral norms; regardless, sex dates and anonymous sex happen. If you, like many people, engage in these sexual practices, it will be up to you to find out what is best for you.
If fucking without a condom is an option for you, then ask yourself first: what does this mean for me? Do I need to do this, and why? Is it simply more fun? What if someone says that they are undetectable: will you, as a person who is HIV negative, fuck with or without condoms? Will you regret it later?
Treatment as prevention only works with dates that you can trust. For some people, trust can be formed through open and casual communication. Disclosing your HIV-positive status is first and foremost a huge leap of faith. One who speaks openly about their treatment and exposure to STIs shows that they take other people’s health and safety seriously. In disclosing your status, you will find out just how familiar your counterpart is with the matter. You might also want to bring your own prior knowledge to the discussion. It is up to you to establish trust and this is only possible with communication.
If you are still feeling uncertain, it’s not a problem. Simply use condoms, or if you are HIV negative, think about taking PrEP! That way you have control over your own prevention strategy (when it comes to HIV).
Maybe you are with someone who identifies as negative and would rather not have sex without a condom. You might have not been tested for a while and it isn’t always clear what has happened since you were. It’s possible that someone is positive and simply doesn’t know their status.
What about STIs? – Condoms can significantly reduce your risk of contracting STIs depending on the STI and the sex practices. Get tested for STIs (every 3 months) and take care of any symptoms that might emerge. Infections that are caught early can be treated easily. If you are into harder sex play, make sure to find out more detailed information.
By the way, the transmission of an STI from an HIV-Negative person to an HIV-Positive person can be an additional health burden. Both people always bear responsibility.
And in the Darkroom? All of these things can’t be discussed in detail. If you want to be absolutely sure, stick with condoms and PrEP! We all know about sex dates and anonymous sex situations where communication about safer sex didn’t work well. Here, treatment as prevention may not be the appropriate method and you should protect yourself and others.
In retrospect, if you still have uncertainties, ask your last date about their status, viral load, and STIs. This works best without accusations. If this doesn’t bring you certainty, you still have the option to get PEP within 48 hours after the encounter.
SHOULD I OUT MYSELF AS POSITIVE BEFORE SEX?
Of course, open communication about everyone’s status before sex would be the best situation. Ideally everyone would speak openly about prevention, their positive or negative status, treatment and STIs, then come to an agreement, and have amazing sex. In this way, all parties would be able to make an informed decision around safety prior to the sexual encounter.
Speaking openly about your HIV status is a huge sign of confidence. “My treatment, your prevention” only works with this level of openness. At the same time, this doesn’t mean that all of the weight of responsibility for safer sex rests upon people who are HIV positive. This contradicts every idea of shared responsibility. The idea of placing responsibility when it comes to sex only on HIV positive individuals also alienates people who are negative: this might simply make them feel like they don’t have agency in the situation.
Legally, it looks like this: if you want to be on the safe side you should inform your sex partner of your own HIV status if you are positive, as courts can interpret sex without condoms as attempted bodily harm. Although HIV-transmission can be eradicated by treatment as prevention, courts still assess the risk differently (especially with regard to whether condoms were used or not). By contrast, people who do not know their status (i.e. HIV positive and untreated individuals) don’t have to fear prosecution.
Anyone who has been previously confirmed to be HIV positive can also be placed in a legally disadvantageous situation. The legal system must change this as quickly as possible and recognize the scientific knowledge that has existed for years! This would encourage more people to test themselves, which in turn could prevent more new infections.
Disclosing your positive status may often result in you experiencing ignorance, fear and rejection. Someone might leave you simply because you are positive. Professional or social discrimination is possible. It is therefore your decision alone, whether you want to out yourself as positive or not.
A TREATED FUTURE?
People who are HIV positive today live long healthy lives, work, and have sex just like people who are HIV negative. Treatment as prevention not only prevents infections, but also brings about the normalization of HIV. Although the proportion of infected people taking ART is significant, the number of new infections among men who have sex with men remains stable, and at a high level: in Germany, this amounts to more than 2,000 people yearly, and in Switzerland more than 250. A significant proportion of these new infections occur only after the onset of the symptoms of the disease. This means that these individuals were infectious and untested for a significant period of time. In recent years as the image of HIV/AIDS has become less shocking, which in itself is a good thing, condom use has also declined.
Safer sex can adapt to the needs and circumstances of each situation, however, condoms continue to provide the best prevention for most people in many moments, especially because of other STIs.
At the same time not everyone knows about treatment as prevention (or at least not in detail). And with PEP and PrEP, there are other options now for protecting oneself from HIV. Not only should the costs be covered for all of these measures so that they are completely accessible, but comprehensive information should also be made readily available. These are political demands that are worth fighting for.
The prices for ART must drop – and if necessary become more regulated – so that they can benefit people in all parts of the world and effectively prevent new infections via treatment as prevention. A world without HIV is possible!
LINKS AND SOURCES
- EKAF statement in english
ternyata.org/books/wisdom/swiss_english.pdf - Sexual Activity Without Condoms and Risk of HIV Transmission in Serodifferent Couples When the HIV-Positive Partner Is Using Suppressive Antiretroviral Therapy (PARTNER study)
jamanetwork.com/journals/jama/fullarticle/253306 - Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER study)
www.thelancet.com/journals/lancet/article/PIIS0140-6736(19)30418-0/fulltext - Zero HIV transmissions in PARTNER 2 study after gay couples had sex 77,000 times without condoms – an undetectable viral load stops HIV
i-base.info/htb/34604 - Information about ART and treatment
www.aidsmap.com/treatmentsdirectory
- HIV specialists (D)
www.hivandmore.de/aerzteverzeichnis - HIV specialists (CH)
www.aids.ch/en/living-with-hiv/advice/specialists.php
- PrEP – our English info about HIV pre exposure prophylaxis
www.lovelazers.org/en/prep-the-before-pill-2 - PEP – our English info about HIV post exposure prophylaxis
www.lovelazers.org/en/pep-the-after-pill - Does the rubber fail the breaking test? — Information about condoms
www.lovelazers.org/en/condoms-pass-the-breaking-test
MORE INFO AND COUNSELING
- Mancheck in Berlin
+49 30 4466 8870
www.mancheck-berlin.de
- Checkpoint in Zürich
+41 44 455 59 10
www.mycheckpoint.ch/de/standorte/zuerich
or at your local German Aids-Hilfe office:
0180 33 19 411 (max. 9ct/min. German landline)
Mon-Fri 9-21h + Sat-Sun 12-14h
and in Switzerland: list of all Aids-Hilfe offices
www.aids.ch/en/about-us/association/antennen.php

Our leaflet/guide texts are subject to constant professional and medical quality control by our Love Lazers Advisory Board
COUNT ON LOVE LAZERS
Love Lazers is an activist group working between Berlin, Zurich and Leipzig. We focus our efforts on cyber and nightlife. Some of us are in gay, discordant relationships (HIV+ and -) and have been educated in the fields of sociology, medicine and law. Some of us have worked for a long time in the areas of prevention and drug work. We’re growing our network and are independent of any specific institutions.
/// You can join us!
/// You can reach us at info@lovelazers.org.
/// You can like us on facebook
© LoveLazers, 2017 – 2019. Translation by Sean, Jonathan and Charles. Thanks for comments, help and impulses: Caro & Doro, Alex, Ivanka, Brenton, Sandra, Tibor, Jérémy, Dario, Oded, Tristan, Sven, Armin, Whit, Andi and Amichai+.
Supported by: mikrodisko boombox, Tuntenhaushoffest, les amies du futur Leipzig, Mancheck.